Employers offering group health coverage that includes any prescription drug benefits must complete two notice and disclosure requirements each year.
Read MoreCarriers are required to pay rebates by Sept. 30, 2022, based on their 2021 MLRs.
Read MoreThe Affordable Care Act requires health insurance issuers and sponsors of self-insured health plans to pay Patient-Centered Outcomes Research Institute (PCORI) fees for plan years ending in 2021. PCORI fees are due July 31st.
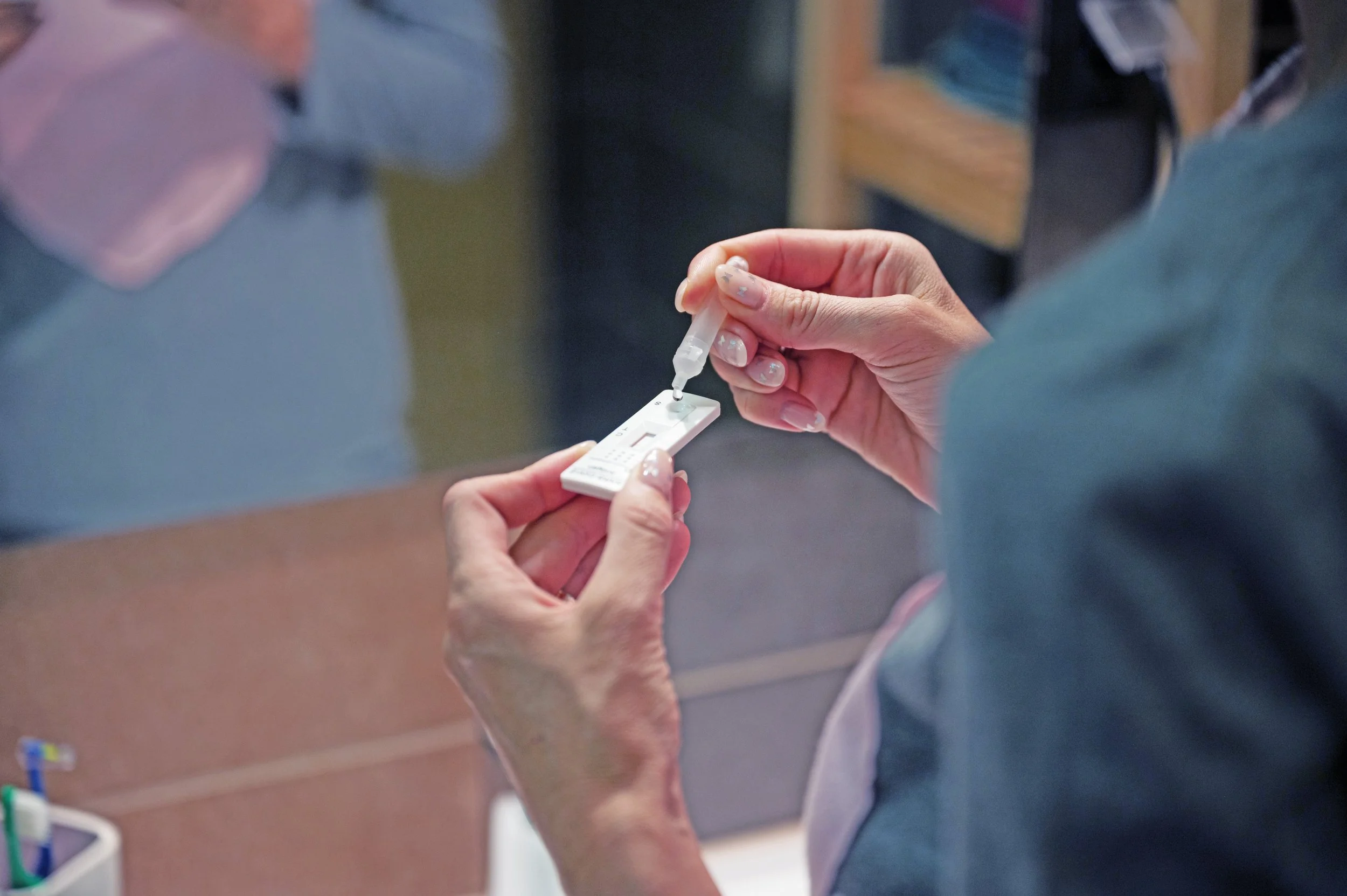
Read MoreBeginning Saturday, January 15, 2022, FDA approved over the counter (OTC) at-home Covid-19 tests are required to be covered by health insurance carriers and group health plans without member cost sharing, preauthorization, or provision by a health care provider.
Read MoreFind out how new legislation under the ARPA will affect employee benefits.
Read MoreIn years past, we would say “Happy Holidays!”. This year, the meaning behind that phrase is different yet powerful.
Read More